GM CASES
Date of admission: 10-08-2021
63 year old male presented to the casualty with history of one episode of involuntary movements of both upper and lower limbs around 11:00 pm, lasting for 5-10 min associated with ictal cry, uprolling of eyeballs and deviation of mouth with ?cheek bite followed by post ictal confusion lasting for 10-15 min.
No H/o involuntary micturition or defecation.
He was taken to a local hospital, where he was administered epitoun and was referred to KIMS (around 1am)
After presentation there was another episode of involuntary movements of both upper and lower limbs, GTCS type with deviation of mouth, lasting for 1-2 mins followed by post ictal confusion for 2-3 min.
He is a known case of seizures since 30 years and on medication carbamazepine 200mg OD & 400mg HS. But he didn't take medication since 2 days.
H/o seizures yearly once or twice for 10 years and was seizure free for the past 10 years.
Known case of type 2 DM since 6 months and on GLIMI 1mg, METFORMIN 500mg
Known case of ?asthma (occasional use of MDI, salbutamol)
Personal history:
Diet - veg
Appetite - normal
Sleep - adequate
Bowel and bladder habits - regular
No addictions
Family history:
No significant history
General examination:
On presentation to us, he was conscious, coherent, co-operative
Moderately built and nourished
No signs of pallor, icterus, cyanosis, clubbing, koilonychia, generalized lymphadenopathy
Vitals at the time of admission:
Temp - 98.4 F
PR - 110 BPM
Bp - 130/80 mm Hg
RR - 18cpm
Spo2 - 98% at room air
GRBS - 166mg/dl
Systemic examination:
CNS:
Speech - normal
No signs of meningeal irritation
Motor & sensory system - normal
Reflexes - normal
Cranial nerves - intact
CVS :
S1, S2 heard
No thrills, Murmurs
Respiratory system:
Position of Trachea - central
NVBS heard
No added sounds
Per abdomen:
Soft, non tender
No palpable masses
Hernial orifices - normal
Bowel sounds heard
Provisional Diagnosis:
Seizures secondary to non compliance to Antiepileptic drugs
Investigations:
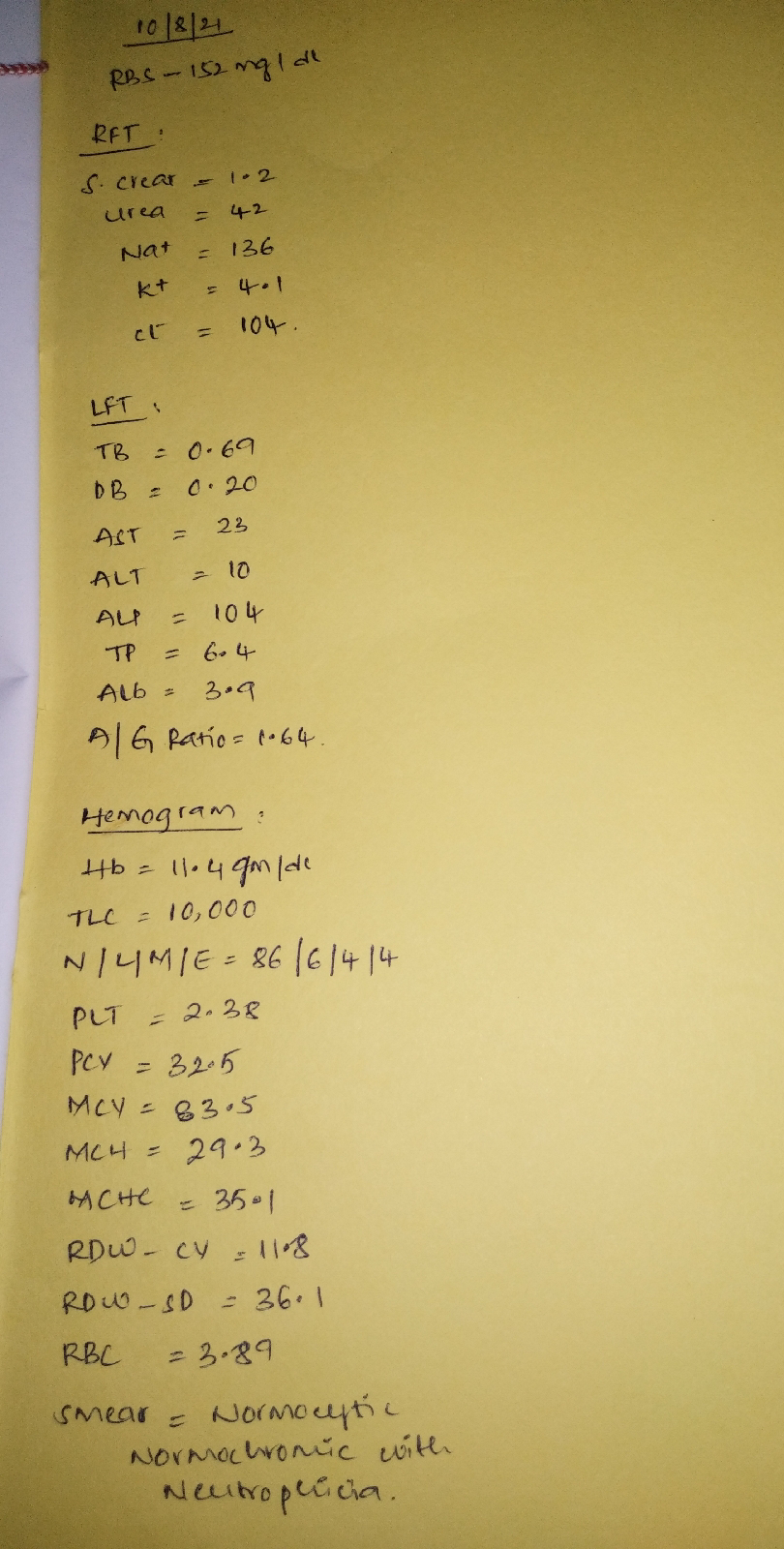
RBS, RFT, LFT, Hemogram:
ECG:
Treatment given:
1. IVF - 1 NS @ 75ml/hr with 1 ampoule of OPTINEURON
2. Inj. LEVIPIL 1gm IV stat
3. Inj. ZOFER 4 mg IV SOS
4. Inj. PAN 40mg IV OD
5. Tab. CARBAMAZEPINE 200mg/PO @ 8:00 am
6. Tab. CARBAMAZEPINE 400mg/PO/HS
7. Tab. GLIMI-M1/PO/OD
8. BP/PR/SPO2 charting 4th hourly
9. GRBS Charting 6th hourly
Discharge summary:
Date: 10-08-21, 3:30 pm
Ward: ICU
Unit: 1
Treating Faculty:
Dr. Pallavi (Internee)
Dr. Avani (Internee)
Dr. Akshitha (Internee)
Dr. Sree Valli (Internee)
Dr. Roshna (Internee)
Dr. Tejaswini (Internee)
Dr. Vijay Dhanush (Internee)
Dr. Vinay (PGY1)
Dr. Shashikala (PGY1)
Dr. Aashitha (PGY2)
Dr. Usha sree (PGY2)
Dr. K. Vaishnavi (PGY2)
Dr. Arjun (ASST PROF)
Dr. Rakesh Biswas (HOD & PROF)
Diagnosis:
Seizures secondary to non compliance to Antiepileptic drugs
Case history:
63 year old male presented to the casualty with history of one episode of involuntary movements of both upper and lower limbs around 11:00 pm, lasting for 5-10 min associated with ictal cry, uprolling of eyeballs and deviation of mouth with ?cheek bite followed by post ictal confusion lasting for 10-15 min.
No H/o involuntary micturition or defecation.
He was taken to a local hospital, where he was administered epitoun and was referred to KIMS (around 1am)
After presentation there was another episode of involuntary movements of both upper and lower limbs, GTCS type with deviation of mouth, lasting for 1-2 mins followed by post ictal confusion for 2-3 min.
He is a known case of seizures since 30 years and on medication carbamazepine 200mg OD & 400mg HS. But he didn't take medication since 2 days.
H/o seizures yearly once or twice for 10 years and was seizure free for the past 10 years.
Known case of type 2 DM since 6 months and on GLIMI 1mg, METFORMIN 500mg
Known case of ?asthma (occasional use of MDI, salbutamol)
Personal history:
Diet - veg
Appetite - normal
Sleep - adequate
Bowel and bladder habits - regular
No addictions
Family history:
No significant history
General examination:
On presentation to us, he was conscious, coherent, co-operative
Moderately built and nourished
No signs of pallor, icterus, cyanosis, clubbing, koilonychia, generalized lymphadenopathy
Vitals at the time of admission:
Temp - 98.4 F
PR - 110 BPM
Bp - 130/80 mm Hg
RR - 18cpm
Spo2 - 98% at room air
GRBS - 166mg/dl
Systemic examination:
CNS:
Speech - normal
No signs of meningeal irritation
Motor & sensory system - normal
Reflexes - normal
Cranial nerves - intact
CVS :
S1, S2 heard
No thrills, Murmurs
Respiratory system:
Position of Trachea - central
NVBS heard
No added sounds
Per abdomen:
Soft, non tender
No palpable masses
Hernial orifices - normal
Bowel sounds heard
Investigations:
MRI Brain:
Few acute lacunar infarcts in bilateral cerebral hemispheres.
Bilateral thin subdural collections over the fronto-parietal convexities.
Treatment given:
1. IVF - 1 NS @ 75ml/hr with 1 ampoule of OPTINEURON
2. Inj. LEVIPIL 1gm IV stat
3. Inj. ZOFER 4 mg IV SOS
4. Inj. PAN 40mg IV OD
5. Tab. CARBAMAZEPINE 200mg/PO @ 8:00 am
6. Tab. CARBAMAZEPINE 400mg/PO/HS
7. Tab. GLIMI-M1/PO/OD
8. BP/PR/SPO2 charting 4th hourly
9. GRBS Charting 6th hourly
Advice at discharge:
1. Tab. CARBAMAZEPINE 200mg/PO/OD
2. Tab. CARBAMAZEPINE 400mg/PO/HS
3. Tab. PAN 40 mg PO/OD
4. Tab. ZOFER 4mg/PO/SOS
5. Tab. GLIMI M1 PO/OD




Comments
Post a Comment