GM CASES
80 year old female, daily wage labourer by occupation came with chief complaints of
Constipation since 3 weeks, pedal edema since 1 week, shortness of breath, cough, abdominal distension and decreased urine output since 3 days.
History of present illness:
She was apparently asymptomatic 3 weeks back. Then c/o difficulty in passing stools (once in 3-4 days) and decreased appetite.
From the past 1 week, patient c/o pedal edema which is of pitting type, extending upto knees. She c/o sob since 3 days, which was sudden in onset, progressed from grade 3 to 4.
C/o cough since 3 days which was productive, mucoid and non blood stained.
History of abdominal distension and decreased urine output since 3 days.
No c/o palpitations, chest pain, syncopal attacks
No history of significant weight loss.
Past history:
History of TB 30 years back and used ATT for 4-6 months
Not a known case of hypertension, diabetes mellitus, asthma, epilepsy, CAD, CVA, Thyroid disorders.
Personal history:
She consumes 90-180 ml of whiskey occasionally and smokes 3-4 chuttas/10 days
Family history:
No significant history
General examination:
Patient is conscious
Pallor +
Icterus +
Pedal edema(B/L) +
No clubbing, cyanosis, koilonychia, generalized lymphadenopathy
Vitals at the time of admission:
Temp- afebrile
PR - 110 BPM
BP - 80/40 mm Hg
Spo2 - 70% at Room air
Systemic examination:
Respiratory system:
BAE+, clear
Wheeze +
Decreased air entry In Right IAA, IMA, ISA
Inspiratory crepts heard in Left IAA, IMA, ISA
CVS:
JVP - raised
S1, S2 heard
No thrills, Murmurs
Per abdomen:
Soft, non tender
No palpable masses
Investigations:
02-08-2021:
Urea - 138
Creat - 3.7
Uric acid - 9.5
Na+ - 131
K+ - 4.3
Cl- - 91
LFT:
TB - 0.90
DB - 0.25
AST - 684
ALT - 508
ALP - 177
TP - 5.8
ALB - 2.7
A/G ratio - 0.90
RBS: 126
CUE:
PT - 25 sec
INR - 1.77
APTT - 49 sec
D dimer: 1000ng/ml
ESR - 10mm/1st hour
RFT:
Review 2d Echo:
04-08-21:
Hemogram:
PT: 25 sec
APTT : 49sec
INR : 1.77
TFT:
05-08-2021:
RFT:
S. Creat - 2.9
Urea - 145
Uric acid - 3.5
Na+ - 135
K+ - 4.1
Cl- - 98
Ca2+ - 10.0
Phosphorus - 6.1
LFT:
TB - 8.32
DB - 3.10
AST - 306
ALT - 210
ALP - 202
TP - 6.1
ALB - 2.7
A/G ratio - 0.80
Chest x-ray:
07-08-2021:
ABG:
RFT:
09-08-2021:
Lung biopsy:
Diagnosis:
AKI secondy to ? Sepsis
With Right heart failure with ?Congestive hepatopathy
With chronic atypical mycobacterium infection
With collapse & fibrosis
With mixed respiratory failure
TREATMENT GIVEN:
Day 1:1. O2 inhalation to maintain SPO2 > or = 90%
2. Inj. LASIX 20mg PO/BD, if SBP >or= 100 mm Hg
3. Inj. NORAD 4ml/hr (↑ or ↓ to maintain MAP >or= 65mm Hg)
4. Inj. THIAMINE 1 amp in 100ml NS IV/TID
5. Inj. PAN 40mg IV/OD
6. Nebulization with DUOLIN 6th hourly, BUDECORT 8th hourly, MUCOMIST 12th hourly
Day 2:
Same treatment followed
( Inj. NORAD 6ml/hr
Nebulization with BUDECORT 4th hourly, IPRAVENT 8th hourly, MUCOMIST 12th hourly)
7. Inj. MEROPENEM 500mg IV/BD
8. Inj. VIT-K 10mg IV/OD
9. RT FEEDS: 100ml milk+ 2tsp of protein powder & 50ml free water 4th hourly added
Day 3:
Same treatment followed
( Inj. NORAD 4ml/hr
Nebulization with BUDECORT 2nd hourly, MUCOMIST 6th hourly)
Tab. SHELCAL 500mg RT/OD
Tab. FEBUXOSTAT 40mg RT/OD
Inj. CLEXANE 20mg SC/OD added
Day 4:
Same treatment followed except Inj.NORAD, Inj. VIT- K
Tab. ITRACONAZOLE 100mg PO/OD added
Day 5:
Same treatment followed except Tab. SHELCAL, Tab. FEBUXOSTAT
Tab. UDILIV 200mg RT/OD added
Day 6:
Same treatment followed.
Inj. NORAD @6ml/hr
Syp. LACTULOSE 15ml/RT/BD added
08-08-2021:
Today morning around 9:30 am, B/L pupils dilated, non reactive to light, saturations are not maintained and BP is also not recordable. Immediate CPR was initiated and continued for 6 cycles. After 6 cycles ECG showed flat line that confirmed death.
Time of death: 08/08/2021, @ 10:10 am
Immediate cause of death:
Refractory hypotension secondary to sepsis, respiratory failure
Antecedent cause of death:
AKI secondary to sepsis induced
With right heart failure with Congestive hepatopathy
With chronic atypical mycobacterium Infection
With chronic fibrosis and collapse of right middle lobe and lingular segment
DEATH SUMMARY:
Date: 08-08-2021
Unit : 1
Ward : ICU
Treating faculty:
Dr. Pallavi (Internee)
Dr. Avani (Internee)
Dr. Akshitha (Internee)
Dr. Sree Valli (Internee)
Dr. Roshna (Internee)
Dr. Tejaswini (Internee)
Dr. Vijay Dhanush (Internee)
Dr. Vinay (PGY1)
Dr. Shashikala (PGY1)
Dr. Aashitha (PGY2)
Dr. Usha sree (PGY2)
Dr. K. Vaishnavi (PGY2)
Dr. Arjun (ASST PROF)
Dr. Rakesh Biswas (HOD & PROF)
Diagnosis:
AKI secondy to ? Sepsis
With Right heart failure with ?Congestive hepatopathy
With chronic atypical mycobacterium infection
With collapse & fibrosis
With mixed respiratory failure
Case history:
80 year old female, daily wage labourer by occupation came with chief complaints of
Constipation since 3 weeks, pedal edema since 1 week, shortness of breath, cough, abdominal distension and decreased urine output since 3 days.
History of present illness:
She was apparently asymptomatic 3 weeks back. Then c/o difficulty in passing stools (once in 3-4 days) and decreased appetite.
From the past 1 week, patient c/o pedal edema which is of pitting type, extending upto knees. She c/o sob since 3 days, which was sudden in onset, progressed from grade 3 to 4.
C/o cough since 3 days which was productive, mucoid and non blood stained.
History of abdominal distension and decreased urine output since 3 days.
No c/o palpitations, chest pain, syncopal attacks
No history of significant weight loss.
Past history:
History of TB 30 years back and used ATT for 4-6 months
Not a known case of hypertension, diabetes mellitus, asthma, epilepsy, CAD, CVA, Thyroid disorders.
Personal history:
She consumes 90-180 ml of whiskey occasionally and smokes 3-4 chuttas/10 days
Family history:
No significant history
General examination:
Patient is conscious
Pallor +
Icterus +
Pedal edema(B/L) +
No clubbing, cyanosis, koilonychia, generalized lymphadenopathy
Vitals at the time of admission:
Temp- afebrile
PR - 110 BPM
BP - 80/40 mm Hg
Spo2 - 70% at Room air
Systemic examination:
Respiratory system:
BAE+, clear
Wheeze +
Decreased air entry In Right IAA, IMA, ISA
Inspiratory crepts heard in Left IAA, IMA, ISA
CVS:
JVP - raised
S1, S2 heard
No thrills, Murmurs
Per abdomen:
Soft, non tender
No palpable masses
Investigations:
MRI - BRAIN:
1. FEW ACUTE LACUNAR INFARCTS IN BILATERAL CEREBRAL HEMISPHERES
2. BILATERAL THIN SUBDURAL COLLECTIONS OVER THE FRONTO- PARIETAL CONVEXITIES
2D ECHO:
- NO RWMA, MILD LVH + (1.2CM)
- SEVERE TR+ WITH MODERATE PAH (50+10= 60 MM HG)
- MILD TO MODERATE AR+, TRIVIAL MR+
- SCLEROTIC AV, NO AS/MS
- GOOD LV SYSTOLIC FUNCTION
- EF=58
- DIASTOLIC DYSFUNCTION+
- MINIMAL PE+
- IVC SIZE (2.15CM) DILATED
- DILATED RA, RV, IVC
USG ABDOMEN:
IMPRESSION:
1. BILATERAL GRADE 1-2 RPD
2. MILD ASCITIS
3. DIFFUSE EDEMA OF SKIN & SUBCUTANEOUS TISSUE OF ANTERIOR ABDOMINAL WALL.
Lung biopsy:
No growth after 48hrs of aerobic incubation.
02-08-2021:
ABG:
pH - 7.165
pCO2 - 60.4
pO2 - 79.0
HCO3- - 20.9
HCO3-(st) - 18.8
RFT:
Urea - 138
Creat - 3.7
Uric acid - 9.5
Na+ - 131
K+ - 4.3
Cl- - 91
LFT:
TB - 0.90
DB - 0.25
AST - 684
ALT - 508
ALP - 177
TP - 5.8
ALB - 2.7
A/G ratio - 0.90
CUE:
Color - pale yellow
Appearance - clear
Reaction - acidic
Sp. Gravity - 1.010
Albumin - +
Sugar, bile salts, bile pigments - Nil
Pus cells - 3-4
Epithelial cells - 2-3
RBC, crystals, casts - Nil
Amorphous deposits - absent
ABG:
pH - 7.166
pCO2 - 57.5
pO2 - 50.9
HCO3- - 20.0
HCO3-(st) - 17.9
03-08-2021:
ABG:
pH - 7.129
pCO2 - 61.8
pO2 - 69.5
HCO3- - 19.7
HCO3-(st) - 17.1
APTT: 49sec
PT: 24 sec
INR : 1.77
RFT:
S.creat -4.1
Urea - 169
Uric acid - 10.2
Na+ - 130
K+ - 4.9
Cl- - 92
Ca+2 - 8.2
Phosphorus - 7.9
Hemogram:
Hb - 8.3
TLC - 25000
N/L/M/E - 85/7/6/2
PCV - 28.0
MCV - 86.2
MCH - 25.5
MCHC - 29.6
RDW-CV - 27.4
RDW-SD - 82.9
RBC Count - 3.25
Platelet count - 1.0
Smear - normocytic normochromic with neutrophilic leukocytosis
Dengue NS1 antigen, IgG, IgM : negative
D-DIMER : 1000ng/ml
ESR : 10mm/1st hour
ABG:
pH - 7.183
pCO2 - 45.4
pO2 - 97.9
HCO3- - 16.4
HCO3-(st) - 15.8
04-08-2021:
ABG:
pH - 7.251
pCO2 - 53.5
pO2 - 88.1
HCO3- - 22.7
HCO3-(st) - 21.2
Hemogram:
Hb - 7.0
TLC - 19200
N/L/M/E - 82/9/5/4
PCV - 22.7
MCV - 79.6
MCH - 24.6
MCHC - 30.8
RDW-CV - 26.9
RDW-SD - 75.3
RBC Count - 2.85
Platelet count - 1.1
Smear - normocytic normochromic with neutrophilic leukocytosis
PT : 25 sec
APTT : 49sec
INR : 1.77
LFT:
TB - 2.50
DB - 1.05
AST - 1.052
ALT - 477
ALP - 229
TP - 6.0
Albumin - 2.8
A/G ratio - 0.86
RFT :
S. Creat - 2.9
Urea - 138
Uric acid - 4.9
Na+ - 136
K+ - 4.1
Cl- - 99
Ca2+ - 9.0
Phosphorus - 5.7
TFT:
T3 - 0.39
T4 - 3.53
TSH - 1.93
05-08-2021:
Hemogram:
Hb - 6.5
TLC - 17700
N/L/M/E - 74/16/5/5
PCV - 21.7
MCV - 78.9
MCHC - 23.6
MCHC - 30.0
RDW-CV - 25.1
RDW-SD - 69.4
RBC Count - 2.75
Platelet count - 1.12
Smear : normocytic normochromic anemia with leukocytosis and thrombocytopenia
RFT:
S. Creat - 3.5
Urea - 188
Uric acid - 4.9
Na+ - 136
K+ - 4.5
Cl- - 101
Ca2+ - 9.6
Phosphorus - 7.0
ABG:
pH - 7.12
pCO2 - 66.2
pO2 - 102
HCO3 -21.6
St. HCO3 -19.7
06-08-2021:
ABG:
pH -7.192
pCO2-64.5
pO2 -122
HCO3 -23.8
St. HCO3 -21.4
LFT:
TB - 8.32
DB - 3.10
AST - 306
ALT - 210
ALP - 202
TP - 6.1
Albumin - 2.7
A/G ratio - 0.80
RFT :
S. Creat - 2.9
Urea - 145
Uric acid - 3.5
Na+ - 135
K+ - 4.1
Cl- - 98
Ca2+ - 10.0
Phosphorus - 6.1
Hemogram:
Hb - 6.3
TLC - 22000
N/L/M/E - 70/20/8/2
PCV - 21.4
MCV - 76.7
MCHC - 22.6
MCHC - 29.4
RDW-CV - 24.0
RDW-SD - 62.3
RBC Count - 2.78
Platelet count - 1.3
Smear : normocytic normochromic anemia with leukocytosis and mild thrombocytopenia
PT: 18sec
INR : 1.3
APTT: 37 sec
07-08-2021:
ABG:
pH- 7.110
pCO2 - 98.5
pO2 - 52.5
HCO3 - 29.9
St HCO3 - 23.2
ABG:
pH - 7.179
pCO2 - 67.9
pO2 - 312
HCO3 - 24.3
St. HCO3 - 21.0
ABG:
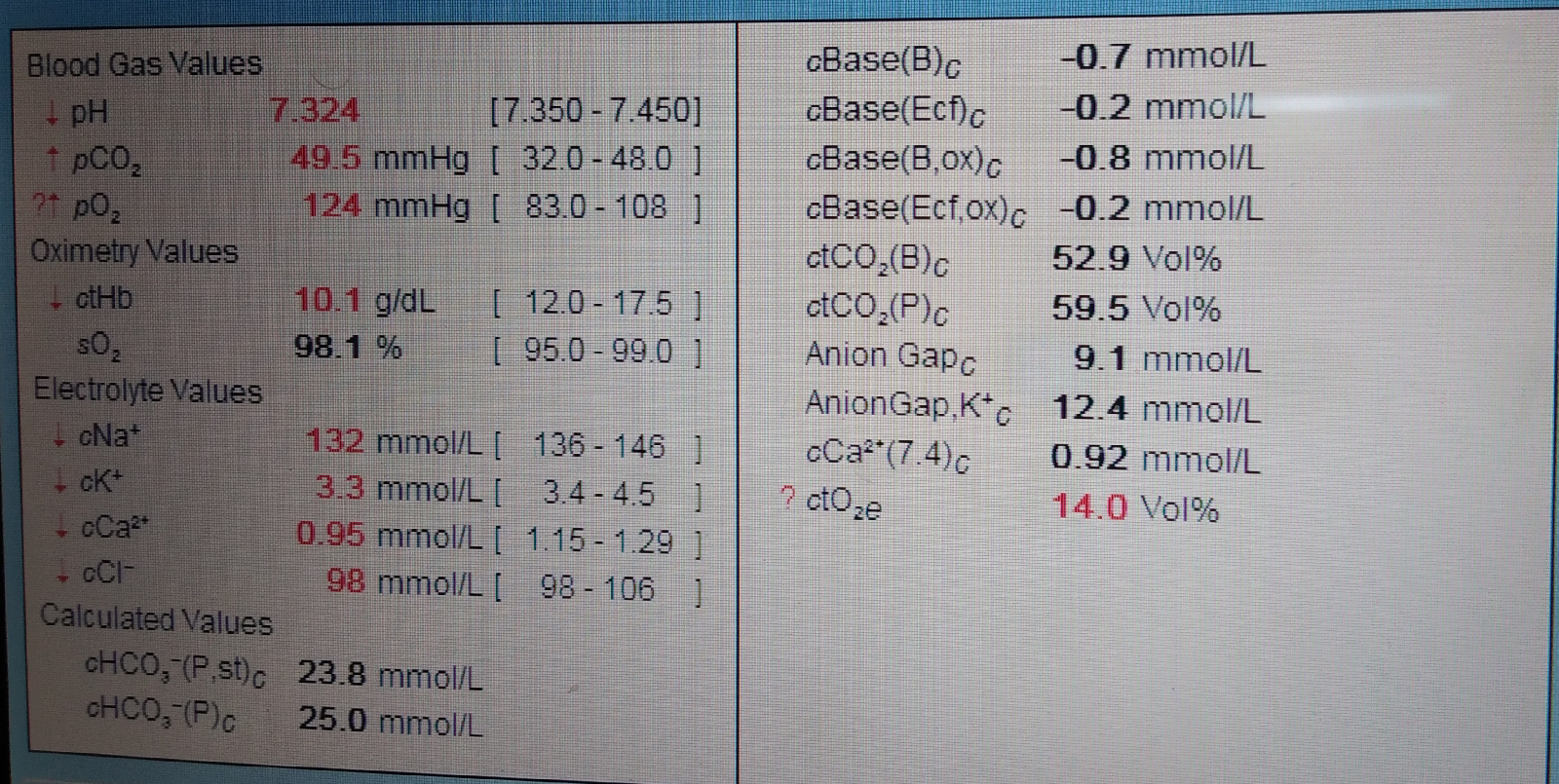
pH - 7.324
pCO2 - 49.5
pO2 - 124
HCO3 - 25 .0
St. HCO3- 23.8
RFT:
Sr. Creat - 2.7
Urea - 108
Uric acid - 2.9
Na+ - 130
K+ - 3.9
Cl- - 95
Ca+2 - 8.7
Phosphorus - 5.8
Hemogram:
Hb - 9.1
TLC - 19400
N/L/M/E - 78/16/5/1
PCV - 29.1
MCV - 80.4
MCH- 25.1
MCHC - 31.3
RDW-CV - 24.7
RDW-SD- 69.6
RBC count- 3.62
Platelet count- 1.5
Smear - dimorphic anemia with leukocytosis
Treatment given:
Day 1:
1. O2 inhalation to maintain SPO2 > or = 90%
2. Inj. LASIX 20mg PO/BD, if SBP >or= 100 mm Hg
3. Inj. NORAD 4ml/hr (↑ or ↓ to maintain MAP >or= 65mm Hg)
4. Inj. THIAMINE 1 amp in 100ml NS IV/TID
5. Inj. PAN 40mg IV/OD
6. Nebulization with DUOLIN 6th hourly, BUDECORT 8th hourly, MUCOMIST 12th hourly
Day 2:
Same treatment followed
( Inj. NORAD 6ml/hr
Nebulization with BUDECORT 4th hourly, IPRAVENT 8th hourly, MUCOMIST 12th hourly)
7. Inj. MEROPENEM 500mg IV/BD
8. Inj. VIT-K 10mg IV/OD
9. RT FEEDS: 100ml milk+ 2tsp of protein powder & 50ml free water 4th hourly added
Day 3:
Same treatment followed
( Inj. NORAD 4ml/hr
Nebulization with BUDECORT 2nd hourly, MUCOMIST 6th hourly)
Tab. SHELCAL 500mg RT/OD
Tab. FEBUXOSTAT 40mg RT/OD
Inj. CLEXANE 20mg SC/OD added
Day 4:
Same treatment followed except Inj.NORAD, Inj. VIT- K
Tab. ITRACONAZOLE 100mg PO/OD added
Day 5:
Same treatment followed except Tab. SHELCAL, Tab. FEBUXOSTAT
Tab. UDILIV 200mg RT/OD added
Day 6:
Same treatment followed.
Inj. NORAD @6ml/hr
Syp. LACTULOSE 15ml/RT/BD added
Death summary:
80 year old female, daily wage labourer by occupation came with chief complaints of
Constipation since 3 weeks, pedal edema since 1 week, shortness of breath (grade 4), cough, abdominal distension and decreased urine output since 3 days. She presented to the hospital in altered state with saturation at room air was 65-68% and with high flow oxygen saturation was 85-90%. Her echo showed right heart failure and kept on high flow oxygen since then. She was drowsy since the admission and 1 transfusion has been done(HB -5.3gm/dl) and due to no urine output 3 sessions of Hemodialysis has been done and due to falling saturation (ABG showed pO2 around 75) patient has been intubated by ET 7.0 on 7th Aug @ 9:15 am and since then Patient is kept on ACMV mode with
Fio2 - 50%
RR - 14cpm
VT - 380
Today morning around 9:30 am, B/L pupils dilated, non reactive to light, saturations are not maintained and BP is also not recordable. Immediate CPR was initiated and continued for 6 cycles. After 6 cycles ECG showed flat line that confirmed death.
Time of death: 08/08/2021, @ 10:10 am
Immediate cause of death:
Refractory hypotension secondary to sepsis, respiratory failure
Antecedent cause of death:
AKI secondary to sepsis induced
With right heart failure with Congestive hepatopathy
With chronic atypical mycobacterium Infection
With chronic fibrosis and collapse of right middle lobe and lingular segment
































Comments
Post a Comment